Preventable Health Care Harm Is a Public Health Crisis
Preventable harm in health care is a public health crisis, with estimates placing it as a leading cause of death in United States.
The National Patient Safety Foundation calls on health care leaders and policymakers to initiate a coordinated public health response to improve patient safety and drive the collective work needed to ensure that patients and those who care for them are free from preventable harm. Such an approach has already contributed to significant reductions in health care-associated infections.
 NPSF believes that a public health response-one that draws on the experience and expertise of public health professionals and public health organizations-will accelerate progress in the prevention of harm and establish the critical infrastructure needed to address this challenge across the US health care system consistently.
NPSF believes that a public health response-one that draws on the experience and expertise of public health professionals and public health organizations-will accelerate progress in the prevention of harm and establish the critical infrastructure needed to address this challenge across the US health care system consistently.
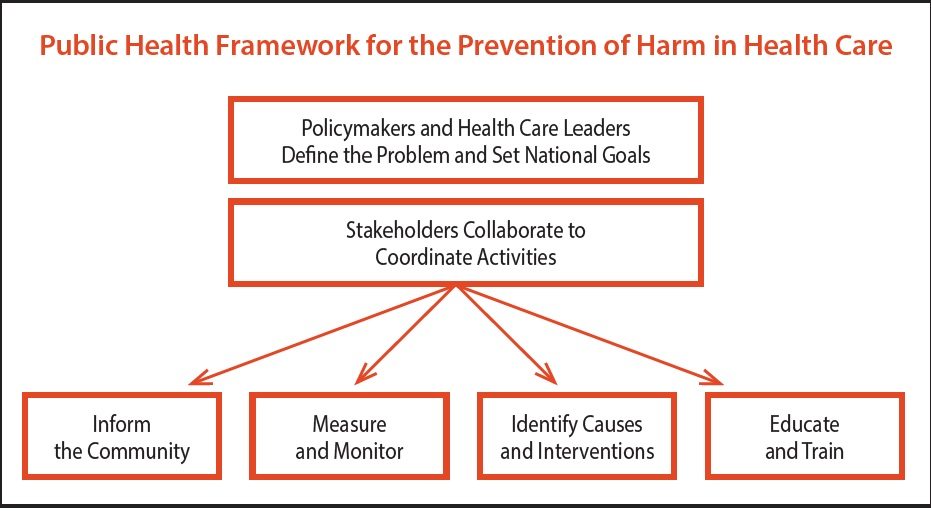
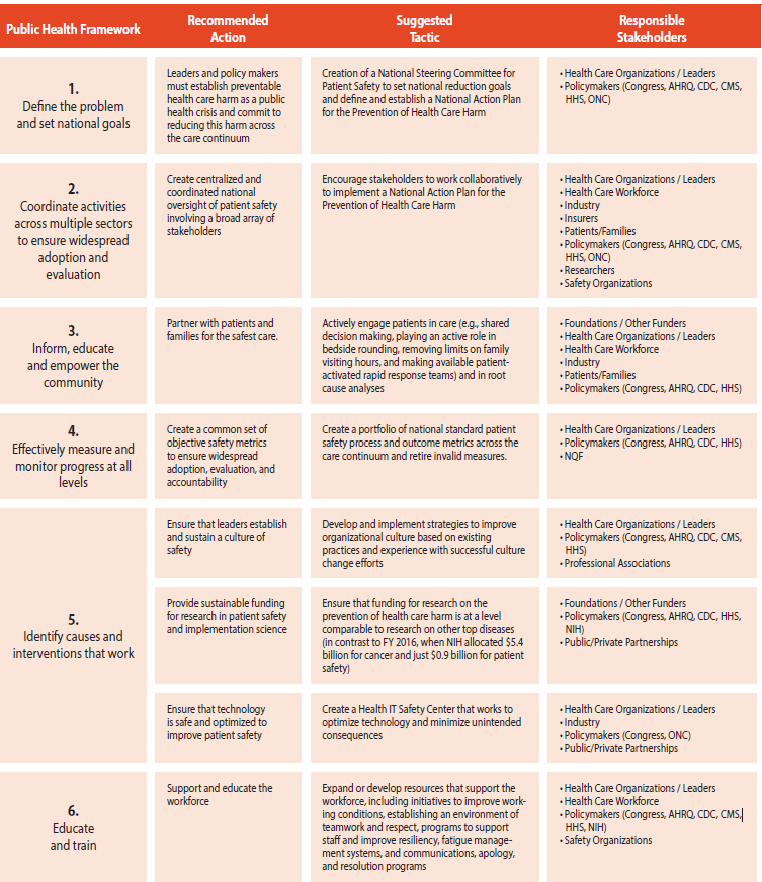
Building on successful efforts to reduce heal care associated infections and taking advantage of critical lessons learned, NPSF proposes the following public health framework to guide efforts. This evidence based approach identifies effective interventions for effective propagation across the health care system.
NPSF urges greater collaboration among all stakeholders to address preventable health care harm and recommends widespread adoption of their public health framework to guide collective efforts. Too often, efforts to blame individuals and organizations for preventable harm diverts attention and resources away from a more effective and sustainable collective response.
Problem Statement
Most care provided in the United States is high quality and safe, but technical treatment advances also create new or expanded opportunities for unintentional, preventable harm to occur. As outlined in the National Patient Safety Foundation report Free from Harm: Accelerating Patient Safety Improvement Fifteen Years after To Err Is Human, errors and injuries that occur during
care may cause significant mortality and morbidity, and can undermine patients’ quality of life.
Efforts to improve patient safety have been ongoing for several decades, but the scale of improvement has been limited and inconsistent, with some organizations succeeding more than others. Some health care organizations have been able to successfully implement improvement strategies while others have been unable to introduce these same interventions or replicate the results.
Health care benefits from dedicated workforce, but the systems and conditions that support safe care practice often falls short. When preventable harm occurs, a host of organizational factors often contributed to the outcome, many outside the control of any one person. A preoccupation with blame has distracted attention away from addressing the broader systemic issues at hand.
Meaningful advancement in patient safety requires a shift from reactive, piecemeal interventions occurring at individual organizations to a coordinated system-wide effort geared at providing safe care delivery across all aspects of care. Also needed is less finger-pointing and more collaboration. All health care stakeholders should work together to anticipate risk and uniformly apply system wide safety processes across the care continuum. Critical, too, is support for health care professionals and other members of the workforce, as well as engagement of patients and families. This reflects a key lesson of the past decade: Most improvement initiatives only succeed when leadership, culture, and patient engagement are fully aligned with the objective of greater safety. A public health approach and our framework emphasize each of these essential components.
Using an integrated, evidence-based approach, public health seeks to ensure protection from — and prevention of — harm to the entire population. This approach, as outlined in their framework, identifies sources of preventable harm — in the case of patient safety, protection from harm related to health care — and then deploys coordinated prevention efforts (e.g., event surveillance and reporting, promotion of behavior change, and evidence-based interventions). It also would provide a structured method for integrating systems and the adoption of key patient safety and implementation science principles.
The advantages of a public health response are visible in work by the US Department of Health and Human Services and the Centers for Disease Control and Prevention to reduce health care–associated infections (HAIs). Established in 2008, the Federal Steering Committee for the Prevention of Health Care–Associated Infections united efforts of the US Departments of Health and Human Services, Labor, and Veterans Affairs.
It released the National Action Plan to Prevent Health Care–Associated Infections in 2009 to coordinate and guide efforts among agencies and stakeholders towards the elimination of HAIs and to set specific reduction goals. The most recent progress report documents significant reductions, including a 50 percent decrease in central line–associated bloodstream infections.
Each of us will be patients during our lives. By extension, all members of society have a stake in improving the safety of our health care system. Similarly, successful implementation of a public health response to prevent health care harm requires coordination and partnership among all stakeholders, including government agencies, health care organizations, insurers, foundations, industry and other private sector organizations, as well as policymakers, patients and families, health care leaders, health professionals, and other members of the health care workforce.
Call To Action
By initiating a public health response, health care leaders and policymakers can accelerate progress in patient safety and establish the infrastructure needed to ensure that patients and those who care for them are free from preventable harm across the health care system.
Article comes from NPSF